The Definitive Scientific Approach to Weight Loss with PCOS
The Calorie Myth and the Hormonal Reality
Weight loss with PCOS can be challenging due to hormonal imbalances, but it can be achieved through a combination of a low-glycemic index diet, regular exercise, and managing stress.
The scientific consensus is clear: the only sustainable and effective path to weight loss with PCOS is to shut down this insulin-androgen cycle by improving your Insulin Sensitivity and achieving metabolic resilience. This is why a simple calorie-restricted diet often fails; it addresses the symptom (weight) but ignores the driver (hormones and cell signaling).
For millions of individuals with Polycystic Ovary Syndrome (PCOS), the standard weight loss advice—”eat less, move more”—is not just ineffective, it is profoundly frustrating. This common advice incorrectly treats weight gain as a simple energy balance issue, ignoring the underlying hormonal and metabolic dysfunctions that define the syndrome.
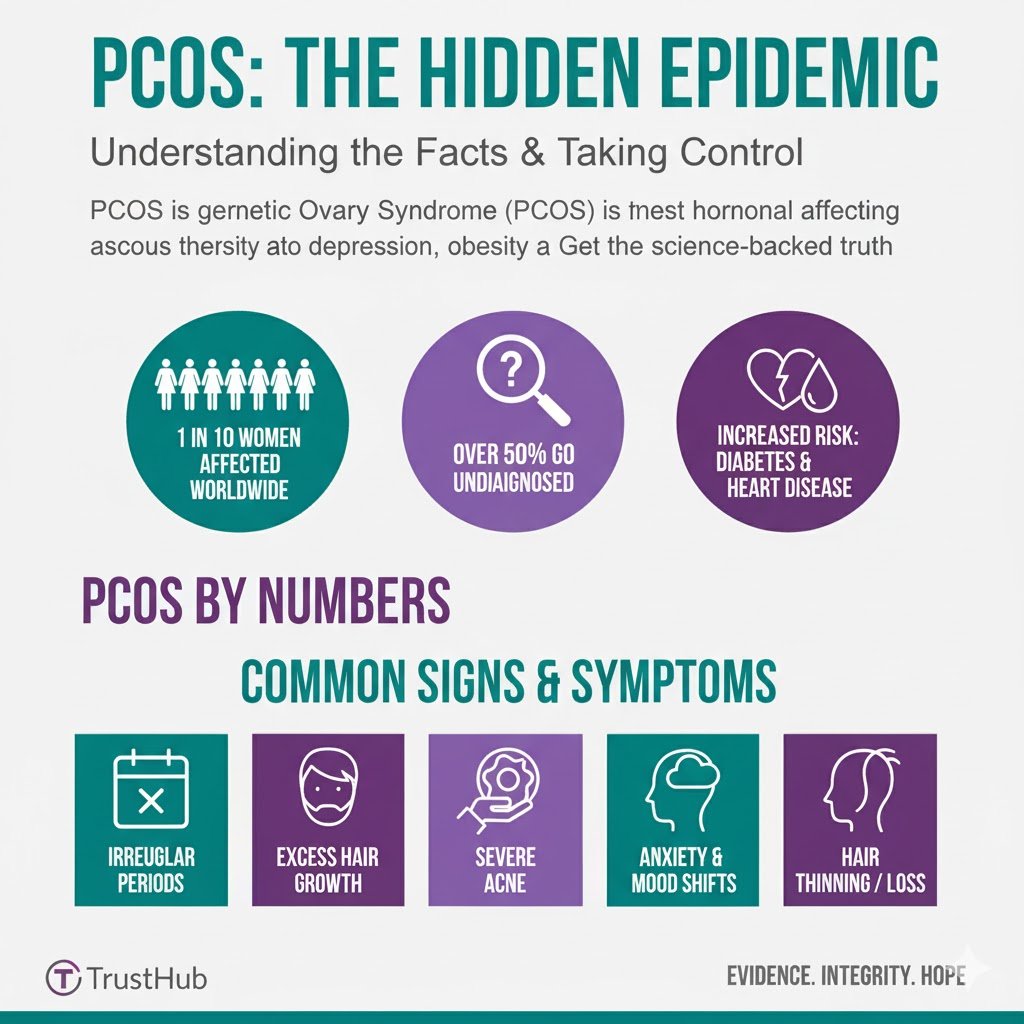
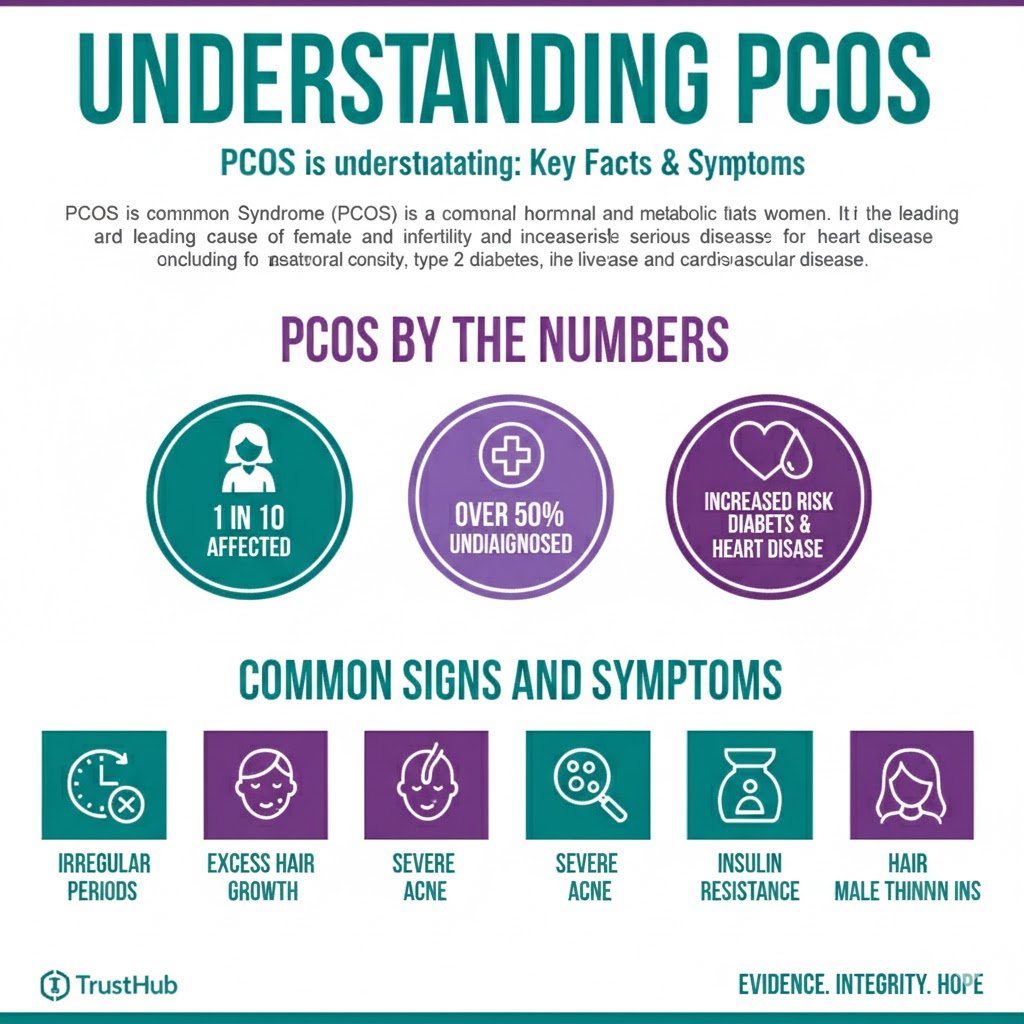
PCOS is the most common endocrine disorder in women of reproductive age, affecting approximately 5–10% globally, and over 50% of those women struggle with overweight or obesity.
The core issue is not a lack of willpower, but a complex metabolic cascade rooted in Insulin Resistance (IR). Therefore, the path to sustainable weight management PCOS is not through restrictive dieting, but through targeted metabolic and hormonal regulation.
The TrustHub methodology bypasses the noise of fad diets and focuses solely on the evidence. The evidence demonstrates that the most effective strategy for weight loss with PCOS is achieving metabolic resilience by directly improving cellular sensitivity to insulin.
Understanding the Metabolic Root Cause: The Insulin-Androgen Cycle
The Link Between Insulin Resistance and PCOS
Insulin Resistance is the critical component that links weight struggles with PCOS symptoms.
A. What is Insulin Resistance (IR)?
Insulin is a vital hormone produced by the pancreas. Its primary job is to act as a “key” that unlocks cell membranes (muscle, fat, and liver) to allow glucose (sugar) from the bloodstream to enter and be used for energy or stored.
In Insulin Resistance, these cells develop a “key-fob that won’t scan,” meaning they become unresponsive to insulin’s signal.
In response, the pancreas is forced to overcompensate by releasing increasingly large amounts of insulin into the bloodstream, a state known as Hyperinsulinemia.
B. The Vicious Cycle: Hyperinsulinemia and Androgen Production
The excess insulin circulating in the blood does two critical things that block weight loss and exacerbate PCOS symptoms:
- Direct Fat Storage Signal: Insulin is the most powerful fat-storage signal in the body. When insulin levels are chronically high, the body is constantly signaled to store energy, making it physiologically difficult to mobilize and burn stored fat (long-tail keyword: reverse insulin resistance PCOS diet). This creates the common PCOS experience: the body fights fiercely to retain every ounce of fat, even in a calorie deficit.
- Increased Androgen Synthesis: High insulin levels act directly on the ovaries and adrenal glands. This excessive insulin stimulates the ovaries to ramp up production of androgens (male hormones like testosterone). This hormonal imbalance is responsible for the classic PCOS symptoms, including hirsutism, acne, and, critically, anovulation (lack of ovulation), which can lead to infertility.
Statistical Fact: Studies show that 70–95% of overweight individuals with PCOS exhibit Insulin Resistance, compared to 30–75% of lean individuals with PCOS. Targeting IR is a universally applicable intervention.
Scientific Nutrition Strategies: Shifting the Metabolic Landscape
The goal of nutrition for PCOS is not starvation; it is insulin minimization. Every dietary choice must be optimized to blunt glucose spikes and keep baseline insulin levels low.
Quality Over Quantity of Carbohydrates: The Glycemic Load Strategy
For PCOS, the quality of carbohydrates is exponentially more important than the total count.
- Evidence: Research has consistently demonstrated that diets focusing on low-Glycemic Index (GI) and low-Glycemic Load (GL) are superior for improving insulin sensitivity and reducing androgen levels in women with PCOS compared to calorie-matched high-GI diets.
- Actionable Insight: The focus must shift away from refined carbohydrates (which are rapidly converted to glucose, causing large insulin spikes) toward fiber-rich, minimally processed carbohydrates.
- Prioritize: Non-starchy vegetables (e.g., leafy greens, cruciferous vegetables), legumes, and high-fiber, intact whole grains (e.g., steel-cut oats, quinoa, brown rice).
- Refined vs. Whole: A single serving of refined sugar can trigger a greater insulin response than a whole-food, fiber-intact carbohydrate containing the same number of calories.
The Power of Balanced Macronutrients (LTK: Macronutrient balance PCOS)
A successful reverse insulin resistance PCOS diet is inherently high in protein and rich in healthy fats, which are metabolically neutral regarding insulin signaling.
- Protein for Satiety and Metabolism: Protein has a significantly lower impact on blood glucose and insulin compared to carbohydrates. High protein intake is crucial for satiety (reducing the urge to snack, thus lowering overall insulin exposure) and protecting lean muscle mass, which is the primary site for glucose uptake. Aim for 25–35 grams of protein per major meal.
- Healthy Fats and Inflammation: Chronic inflammation is strongly associated with the progression of IR. Fats, particularly those rich in Omega-3 fatty acids (found in fatty fish, walnuts, flaxseeds), are crucial for their anti-inflammatory diet properties. Sourcing fats from avocados, nuts, seeds, and olive oil helps regulate cellular health and reduces the inflammatory signals that worsen IR.
The Importance of Meal Timing and Frequency
- Intermittent Eating Window: Constant snacking or grazing ensures that insulin levels remain elevated throughout the day. Introducing a consistent Time-Restricted Eating (TRE) window (e.g., 10–12 hours) allows the pancreas sufficient rest, leading to a demonstrable improvement in insulin sensitivity over time.
- The Breakfast Priority: Studies indicate that shifting a larger portion of daily calories to breakfast and a smaller portion to dinner can significantly lower insulin and androgen levels in women with PCOS. This aligns with the body’s natural circadian rhythm for glucose metabolism.
Targeted Supplementation and Pharmaceutical Support
Proven Supplements for PCOS Weight Loss and Insulin Control
The TrustHub Vetting Protocol requires that we only recommend interventions supported by robust, peer-reviewed clinical trials.
High-Impact Supplements (LTK: best supplements for PCOS weight loss)
- Inositols (Myo- and D-Chiro-):
- Mechanism: Inositols are B-vitamin-like substances that function as “second messengers,” directly improving how insulin signals within the cell. This improves glucose uptake and reduces androgen production.
- Statistical Fact: Multiple studies, including a 2017 meta-analysis, support that a specific ratio of Myo-Inositol to D-Chiro-Inositol (40:1) is highly effective for improving insulin sensitivity and restoring ovulation in PCOS patients. Dosage typically ranges from 2g to 4g daily.
- Berberine:
- Mechanism: Berberine is an alkaloid compound that activates the AMPK pathway—a cellular energy sensor—which mimics the effects of exercise and is highly effective at improving peripheral insulin sensitivity.
- Comparative Fact: Multiple trials suggest Berberine has a comparable effect to Metformin (a common IR drug) in improving glucose metabolism and lipid profiles, with dosages typically ranging from 500mg to 1500mg daily.
- Vitamin D:
- Deficiency Fact: 67–85% of women with PCOS are deficient in Vitamin D, which is linked to poorer metabolic outcomes. Supplementing Vitamin D improves insulin receptor function and has been associated with a decrease in inflammatory markers.
Pharmaceutical Intervention (Metformin)
While TrustHub emphasizes lifestyle, it is essential to note that the pharmaceutical Metformin (glucophage) remains a cornerstone treatment for IR in PCOS. Metformin works primarily by decreasing glucose production in the liver and increasing peripheral tissue sensitivity to insulin. While effective, lifestyle interventions provide the most sustainable long-term solution.
“While the pharmaceutical Metformin is a cornerstone treatment for improving insulin sensitivity and is commonly prescribed for Weight Loss with PCOS, the TrustHub approach prioritizes the long-term, sustainable mastery achieved through targeted nutritional, supplemental, and behavioral science.”
Lifestyle and Behavioral Interventions
Beyond the Plate: Training and Rest for Metabolic Resilience
The most potent, zero-cost method for improving insulin sensitivity is moving the body.
Exercise as Insulin Sensitizer
- Resistance Training is King: The primary site for glucose disposal is muscle tissue. Resistance training (weight lifting, bodyweight exercises) is the single most effective exercise modality for improving insulin sensitivity. Muscle contraction during strength training increases the absorption of glucose from the blood by up to 50% without requiring an insulin signal.
- Sustainable Activity: Aim for at least 150 minutes per week of moderate-intensity aerobic activity (like brisk walking) and two sessions per week of resistance training. Consistency over intensity is paramount for long-term success.
“For effective Weight Loss with PCOS, Exercise must be strategically utilized: Resistance training, in particular, is the most potent tool to improve insulin sensitivity, directly addressing the core metabolic block.”
Stress and The Cortisol Connection (LSI: Cortisol)
Chronic stress and poor sleep are powerful antagonists to insulin sensitivity.
- Cortisol and Blood Sugar: Stress (physical or psychological) triggers the release of the hormone cortisol. Cortisol’s evolutionary purpose is to raise blood sugar to fuel a “fight or flight” response. Chronic elevation of cortisol leads to chronic elevation of blood sugar, which forces the pancreas to pump out more insulin, directly worsening IR and promoting abdominal fat storage.
- Actionable Strategy: Integrating stress-reducing activities like meditation, consistent sleep hygiene, and restorative movement (like yoga) is not optional; it is a direct metabolic intervention for weight loss with PCOS. Aim for 7–9 hours of quality, uninterrupted sleep per night.
“For Weight Loss with PCOS to be sustainable, managing stress is non-negotiable; chronic stress elevates cortisol, which directly raises blood sugar and forces the pancreas to pump out more insulin, actively worsening Insulin Resistance.”
Building Long-Term Success: The TrustHub Approach
The distinction between dieting dependency and independent mastery lies in behavioral coaching. Sustained success is achieved by integrating the science into non-negotiable, repeatable daily habits, thus building metabolic resilience that lasts beyond any single program.
Conclusion
Weight loss with PCOS is not a moral failing; it is a hormonal puzzle. The evidence-based approach is clear: the most effective, sustainable weight management PCOS strategy involves specifically targeting and reversing Insulin Resistance and the subsequent Hyperinsulinemia.
Focus on whole, unprocessed foods, reduce carbohydrate intake, and prioritize lean protein and healthy fats to challenge weight loss with PCOS.
Physical activity, especially a mix of cardio and strength training, is crucial. Furthermore, adequate sleep and stress management also play a significant role in overcoming the challenge of weight loss with PCOS.
By adopting a low-GL, anti-inflammatory dietary approach, leveraging powerful supplements like Inositol’s, and prioritizing resistance training and high-quality sleep, individuals can effectively shut down the insulin-androgen cycle that has been blocking their progress.
TrustHub is committed to being the authoritative filter in this journey. We provide the scientific framework so you can finally stop dieting and start learning to master your body’s metabolism.
Ready to move from frustration to scientific mastery?
Go to the main menu and Explore our Ultimate Guides or start your personalized metabolic journey with the TrustHub 12-Week Transformation Program for a plan tailored to address your specific insulin sensitivity and hormonal profile.