The cost for every different sort of bariatric surgery varies pretty much. Around big urban areas, this surgery will cost much more and, because of the high populated areas, the surgeons will be in a greater demand and so their fees will be higher.
Insurance for weight loss surgery is a variable amount and differs from a provider to another and, of course, from a country/state to another. First of all, you must find out if your provider covers the type of surgery you are about to have.
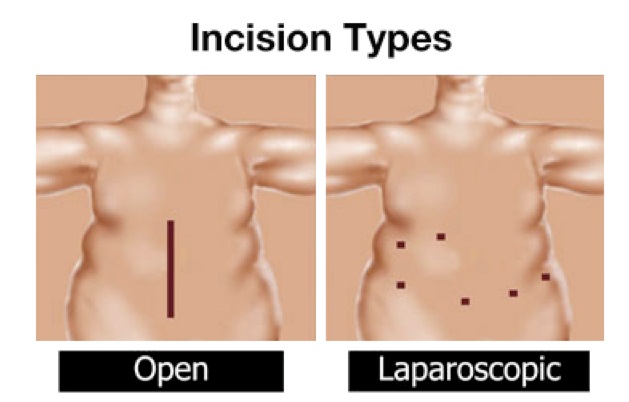
Only few insurance companies will cover the entire bill; most of them will cover only 80% of what is considerate to be “customary”. The base pack for bariatric surgery contains the cost for the hospital facility, for anesthesia, for surgeon and his staff. In USA, the government will pay for three types of bariatric surgery, for people of 65 or older as follow: Laparoscopic adjustable gastric banding, Open and laparoscopic biliopancreatic diversions, The Roux-en-Y bypass. In some USA states, people with low income, are also helped through certain programs to access bariatric surgery.
After surgery, it is possible that you have some additional costs, associated with nutritional supplements, diet and fitness plans, and therapy for modification of your eating behavior. In time, most of the people will need additional surgery to remove excess skin, to lift some of their body areas, to treat fat deposits or to improve muscles condition like: liposuction, breast lift or breast augmentation, abdominal augmentation or face lift. The insurer price for people having diabetes and high blood pressure will be higher because the extra drugs they need while surgery. All those above will not be covered by your insurance except for in rare occasions.
Financial and insurance issues are managed in a personal way by each bariatric surgeon. Anyhow, his office staff should be able to speak to you about your insurance issues. Some clinics might ask the patient to sign a contract that engages him to cover the difference amount of what his insurance company will not cover.
Most of the insurers will request you a letter of medical necessity before agreeing to pay your future bariatric surgery. Insurers might also ask nutritional consultation and psychological evaluation. This medical letter usually must include:
1. Your present weight, your weight history and BMI
2. A history of your dieting efforts, like a physician supervised diet plan and/or six months of office registrations from your supervising doctor
3. A history of your physical exercises at gym
4. A detailed description of your present health condition
5. Your current medication
6. How your daily activities are affected by obesity.